We are pleased to release the schedule for our Fall 2023 seminar series. As in previous series, the seminar will be held via Zoom at 16.00 Central European Time on Thursdays.
To access the Zoom meetings, please join our mailing list here.
24 August
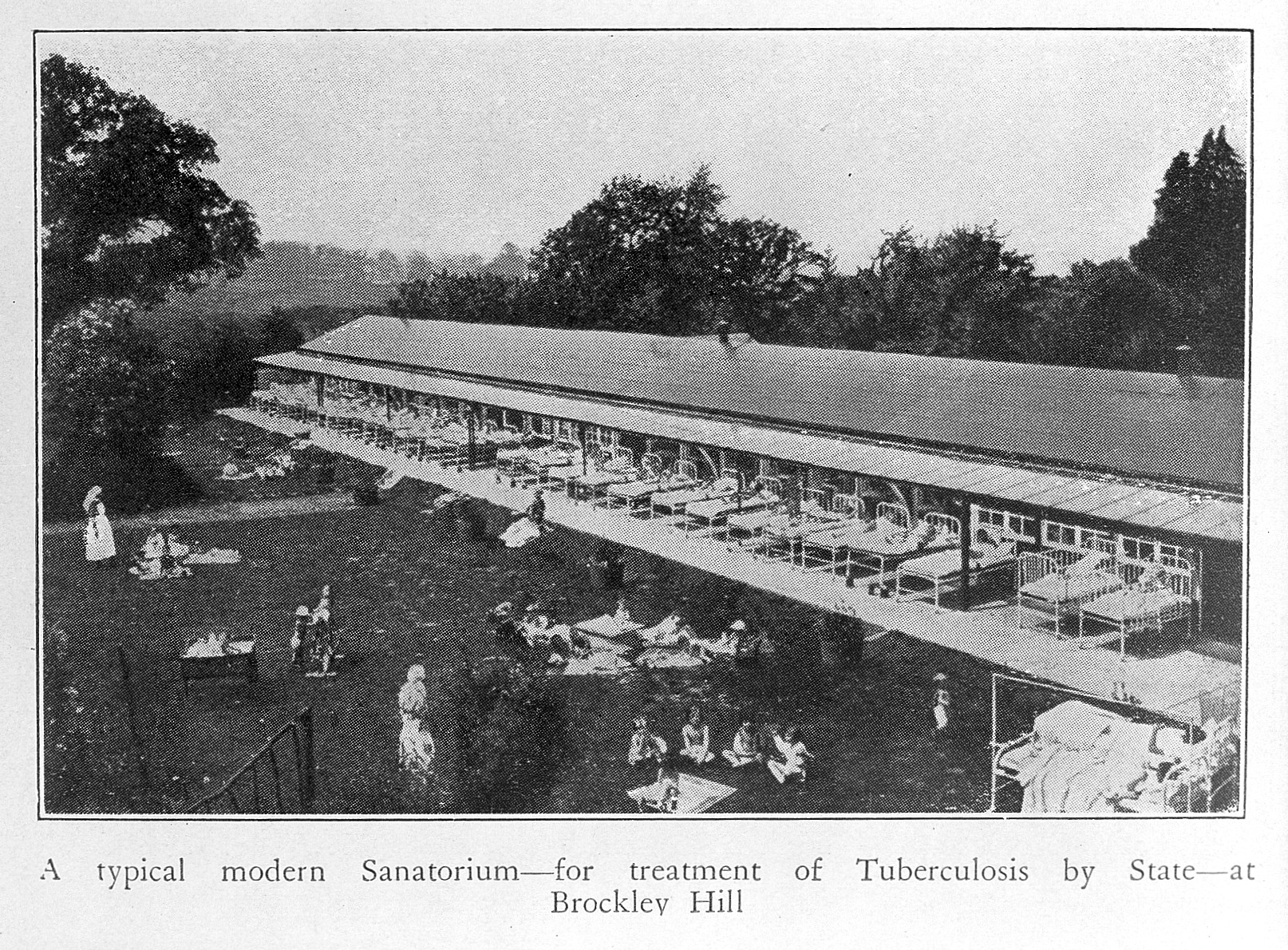
Urban Planning as a Means of Pandemic Prevention – A Look into the RECIPE Project
Eevi Juuti, University of Oulu
7 September – PANSOC MSCA Candidates
Navigating Bias: The Formation of Environmental Collective Perception and Prejudice during San Francisco Plague, 1900
Daijun Liu, Tsinghua University
Title TBA
Maria Dunbar, Oslo Metropolitan University
14 September
On the Move: Fine-Tuning Plague Dispersal in the North Caucasus and Altai-Sayan during Early Bronze Age Human Migrations (3300–2500 BCE)
Rebecca Main, University of Stirling
21 September
The Political Effects of the 1918 Influenza Pandemic in Weimar Germany
Erik Hornung, University of Cologne
12 October
The Cholera Pandemic of 1903–05 and the Influenza Pandemic of 1918 in the Philippines
Francis A. Gealogo, Ateneo de Manila University
19 October
The Grenfell Mission and the 1918 influenza pandemic in Labrador
Uddhav Khakurel, Oslo Metropolitan University
2 November
Geographical inequalities in health during the COVID-19 pandemic in England
Natalie Bennett, Newcastle University
**For our attendees outside of Europe, please note that Central European Summer Time ends on 29 October**
9 November
Age Patterns of Mortality During the Influenza Pandemics of the 20th Century
Lauren Steele, University of Queensland
30 November
Simulating COVID-19’s impact on mental health: An agent-based modelling approach
Kristina Thompson, Wageningen University