New commentary paper in American Journal of Public Health
Gerardo Chowell has written a new commentary piece. You can read it here: Political Determinants of Health: Has COVID-19 Exposed the Worst of It? | AJPH | Vol. Issue (aphapublications.org)
Scientific publications from the researchers involved in PANSOC.
Gerardo Chowell has written a new commentary piece. You can read it here: Political Determinants of Health: Has COVID-19 Exposed the Worst of It? | AJPH | Vol. Issue (aphapublications.org)
We are proud to have published yet another paper from our Social Science Meets Biology | CAS (cas-nor.no) project:
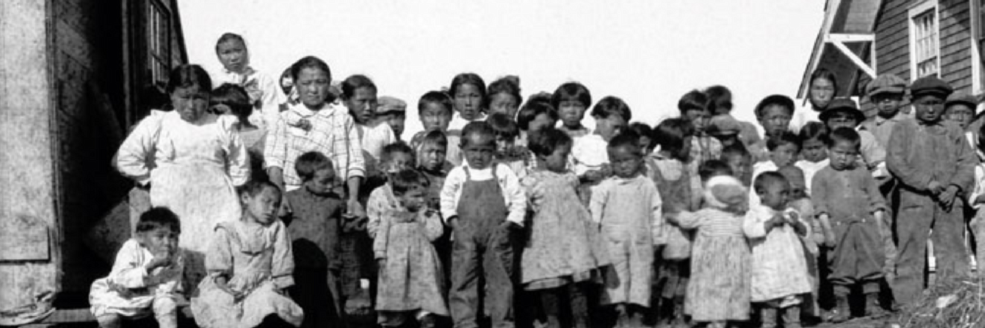
The 1918-20 influenza pandemic devastated Alaska’s Indigenous populations. We report on quantitative analyses of pandemic deaths due to pneumonia and influenza (P&I) using information from Alaska death certificates dating between 1915 and 1921 (n=7,147). Goals include a reassessment of pandemic death numbers, analysis of P&I deaths beyond 1919, estimates of excess mortality patterns overall and by age using intercensal population estimates based on Alaska’s demographic history, and comparisons between Alaska Native (AN) and non-AN residents. Results indicate that ANs experienced 83% of all P&I deaths and 87% of all-cause excess deaths during the pandemic. AN mortality was 8.1 times higher than non-AN mortality. Analyses also uncovered previously unknown mortality peaks in 1920. Both subpopulations showed characteristically high mortality of young adults, possibly due to imprinting with the 1889-90 pandemic virus, but their age-specific mortality patterns were different: non-AN mortality declined after age 25-29 and stayed relatively low for the elderly, while AN mortality increased after age 25-29, peaked at age 40-44, and remained high up to age 64. This suggests a relative lack of exposure to H1-type viruses pre-1889 among AN persons. In contrast, non-AN persons, often temporary residents, may have gained immunity before moving to Alaska.
Responses to the letters on “Mortality in Norway and Sweden during the COVID-19 pandemic 2020 – 22: A comparative study.” in Journal of Infection and Public Health.
We are proud to announce yet another publication from the project PANRISK: Socioeconomic risk groups, vaccination and pandemic influenza (Research Council of Norway grant agreement No 302336)
The paper is joint for with colleagues from the Norwegian Institute of Public Health. You can read the paper here:
We are happy to see that collaboration with PANSOC and PandemicX has led to a new paper: Full article: The 1919–21 influenza pandemic in Greenland (tandfonline.com). This paper is also part of the CAS project on Pandemics and Indigenous Peoples.
Abstract:
In Alaska, the 1918–20 influenza pandemic was devastating, with mortality rates up to 90% of the population, while in other arctic regions in northern Sweden and Norway mortality was considerably lower. We investigated the timing and age-patterns in excess mortality in Greenland during the period 1918–21 and compare these to other epidemics and the 1889–92 pandemic. We accessed the Greenlandic National Archives and transcribed all deaths from 1880 to 1921 by age, geography, and cause of death. We estimated monthly excess mortality and studied the spatial-temporal patterns of the pandemics and compared them to other mortality crises in the 40-year period. The 1918–21 influenza pandemic arrived in Greenland in the summer of 1919, one year delayed due to ship traffic interruptions during the winter months. We found that 5.2% of the Greenland population died of the pandemic with substantial variability between counties (range, 0.1% to 11%). We did not see the typical pandemic age-pattern of high young-adult mortality, possibly due to high baseline mortality in this age-group or remoteness. However, despite substantial mortality, the mortality impact was not standing out relative to other mortality crises, or of similar devastation reported in Alaskan populations.
The paper “Do sociodemographic factors play a role in the relation between COVID-19 infection and obesity? Findings from a cross-sectional study in eastern Oslo” is just published in Journal of Public Health. The author is our former post-doc Margarida Pereira who wrote this paper withing the Reaseach Council of Norway funded project Socioeconomic risk groups, vaccination and pandemic influenza (PANRISK) – OsloMet
Executive summary
The new paper discusses the rising prevalence of overweight and obesity globally and in Norway, highlighting the associated health risks, including an increased susceptibility to severe outcomes from infectious diseases like COVID-19. It explores the social determinants of obesity and how they intersect with the risk of COVID-19 infection, especially in vulnerable populations. The study aims to investigate the relationship between weight status, sociodemographic factors, and COVID-19 infection in Oslo, Norway.
The research, conducted through a web-based survey, examines a sample of individuals from socioeconomically deprived areas with a higher migrant population in Oslo. The survey collected data on weight status, sociodemographic characteristics, and COVID-19 infection status. Statistical analyses, including logistic regression models, were performed to assess the associations between weight status, sociodemographic factors, and COVID-19 infection.
Key findings include:
1. Individuals with overweight or obesity had higher odds of having COVID-19, particularly when adjusted for age, employment status, and other sociodemographic factors.
2. Sociodemographic factors such as age, employment status, district of residence, migrant status, and BMI were significantly associated with the odds of COVID-19 infection.
3. Immigrant women who were young, unemployed, and had overweight or obesity were identified as a high-risk group for COVID-19 infection.
4. The study suggests a syndemic relationship between obesity and COVID-19, emphasizing the need for a multidisciplinary approach to address the complex interplay between biological and social factors contributing to these health outcomes.
Strengths of the study include its large dataset and individual-level data analysis. However, limitations include potential biases related to self-reported height and weight and the small number of confirmed COVID-19 cases in the sample.
In conclusion, the study underscores the importance of considering sociodemographic factors in understanding the relationship between weight status and COVID-19 infection. It advocates for tailored public health interventions targeting vulnerable populations to mitigate the syndemic impact of obesity and COVID-19. Further research is needed to deepen our understanding of these complex interactions and inform more effective public health strategies.
PANSOC Postdoc Maria Dunbar has just published an article in the journal Infectious Disease Modelling. The article reviews different frameworks for conceptualizing how diseases may be transmitted within populations with heterogenous subgroups, called transmission matrices. Early transmission matrices were based on theoretical approaches to population mixing, but these have been supplemented by matrices that have a more empirical basis in, for example, survey data. The paper discusses these different approaches and how common methods have changed over time.
Jessica Dimka, Ben Schneider, and Svenn-Erik Mamelund have recently published a protocol for a systematic review that analyzes evidence on the long-term mental health consequences of historical influenza pandemics. The protocol, published by the Scandinavian Journal of Public Health, is currently available in open access.
The systematic review, which is now in progress, will examine scientific literature that explores whether influenza pandemics from the late 19th century to the early 21st century produced enduring mental illness. The protocol includes a substantial review of relevant literature on the topic that may be of interest to researchers in this area.
In a paper just published in Vaccine: X, Jessica Dimka uses survey data from Oslo to study differences in vaccine uptake and COVID-19 infection between people with chronic health conditions, disabilities, and those without medical risk factors.
Governments took a wide variety of prioritization approaches for COVID-19 vaccination, with some countries or territories giving priority to a people with many types of disabilities and pre-existing medical conditions, and other entities recommending a more narrow prioritization. There is also evidence that people with disabilities are less likely to be vaccinated, either because of vaccine hesitancy or difficulty accessing vaccination sites. In a survey jointly developed by PANSOC and the Pandemic Centre at the University of Bergen, respondents were asked if they had a chronic health condition or disability, whether they planned to take the vaccine, and about disease outcomes.
Analyzing the associations between these data, Dimka found that people with chronic health conditions were more likely to be offered and to accept the vaccine, while individuals with at least one disability were more likely to report a probable COVID case (all in comparison to individuals with no medical risk factors). Reporting probable cases (rather than confirmed) suggests that individuals with disabilities may have had less access to testing or willingness to be tested. The results also indicate that further research is needed to determine potential differences between people with different types of disabilities. In terms of vaccine hesitancy, people with chronic health conditions were less likely to express hesitancy, while people who self-identified as having at least one disability were more likely to be hesitant (than people with no chronic health conditions or disabilities).
Overall, Dimka argues that people with chronic health conditions either exhibited behaviors that might be expected for a group prioritized by public health bodies, or acted in ways accordant with their possible increased risk. In contrast, people with disabilities had little difference from people without risk factors, or slightly worse outcomes in terms of vaccination.
We at PANSOC have been a co-author with other Nordic colleagues writing about the impact of COVID-19 on mortality in Norway and Sweden 2020-22.
The lead author, Per Henrik Zahl, has been interviewed about the paper in Aftenposten: Forskere mener koronatiltak kostet 133 millioner kroner for hvert sparte liv (aftenposten.no)
You can read the paper full here: Mortality in Norway and Sweden during the COVID-19 pandemic 2020 – 22: A comparative study – ScienceDirect
Norway and Sweden picked two different ways to mitigate the dissemination of the SARS-CoV-2 virus. Norway introduced the strictest lockdown in Europe with strict border controls and intense virus tracking of all local outbreaks while Sweden did not. That resulted in 477 COVID-19 deaths (Norway) and 9737 (Sweden) in 2020, respectively.
Weekly number of COVID-19 related deaths and total deaths for 2020-22 were collected as well as weekly number of deaths for 2015-19 which were used as controls when calculating excess mortality. During the first 12-18 months with high rate of virus transmission in the society, excess mortality rates were used as substitute for COVID-19 deaths. When excess mortality rates later turned negative because of mortality displacement, COVID-19 deaths adjusted for bias due to overreporting were used.
There were 17521 COVID-19 deaths in Sweden and 4272 in Norway in the study period. The rate ratio (RR) of COVID-19 related deaths in Sweden vs. Norway to the end of week 43, 2022, was 2.11 (95% CI 2.05-2.19). RR of COVID-19 related deaths vs. excess number of deaths were 2.5 (Sweden) and 1.3 (Norway), respectively. RR of COVID-19 deaths in Sweden vs. Norway after adjusting for mortality displacement and lockdown, was 1.35 (95% CI 1.31-1.39), corresponding to saving 2025 life in Norway. If including all deaths in 2022, RR=1.28 (95% CI 1.24-1.31).
Both COVID-19 related mortality and excess mortality rates are biased estimates. When adjusting for bias, mortality differences declined over time to about 30% higher mortality in Sweden after 30 months with pandemics and at the cost of 12 million € per prevented death in Norway.